transplant rejection
Expand All | Collapse All
Adequacy
- at least 3 fragments
- minimal 3 levels each
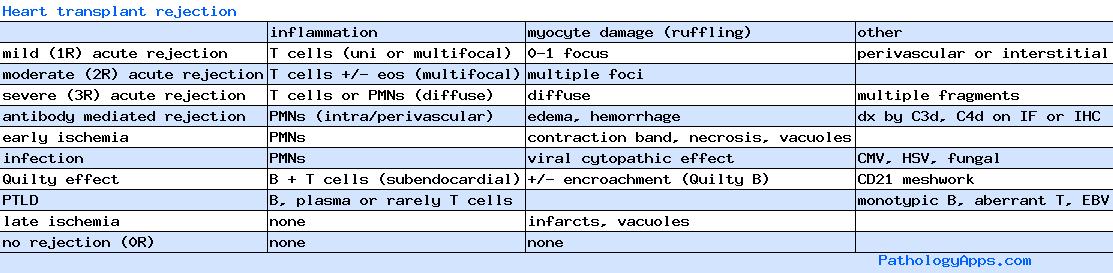
Grading
- Nonrejection
- ischemic injury
- 2004: early (0-6 weeks post-transplant), late (related to allograft CAD)
- 1990: A (0-3 weeks post-transplant), B (late ischemia)
- histology
- early: contraction band, necrosis, myocyte vacuolization, mixed inflammatory infiltrate
- late: vacuolization, microinfarcts
- ischemia predominance over inflammation
- quilty effect
- 1990 A: endocardium only, no myocyte encroachment
- 1990 B: myocyte encroachment
- subyping A vs B has no clinical significance
- B cells, plasma cells
- background fibrosis and vascularity favors quilty
- CD21 highlights follicular dendritic cell network
- infection
- lymphoproliferative disorder
- ischemic injury
- acute cellular rejection
- 0R: no acute cellular rejection
- no mononuclear infiltrate
- no myocyte damage
- 1R: mild acute rejection
- mononuclear infiltrate (perivascular, interstitial)
- up to 1 focus of myocyte damage
- encompasses 1990 grade 1A, 1B, 2
- 1A: focal infiltrate, no myocyte damage
- 1B: diffuse infiltrate, no myocyte damage
- 2: focal infiltrate with myocyte damage
- 2R: moderate acute rejection
- multiple mononuclear infiltrates with myocyte damage
- may have eosinophils
- foci may be in same or different fragments
- encompasses 1990 grade 3A
- 3R: severe acute rejection
- diffuse inflammation with myocyte damage
- mononuclear or PMNs
- in multiple fragments
- encompasses 1990 grade 3B, 4
- 0R: no acute cellular rejection
- Humoral / antibody-mediated rejection (AMR)
- histology
- endothelial cell swelling
- intravascular macrophages
- edema, hemorrhage
- PMNs within and around small vessels
- confirmatory IF/IHC
- IF: C3d, C4d deposition in capillaries
- IHC: C3d, CD68
- donor-specific antibodies in serum
- AMR0
- no histologic or immunopathologic features of AMR
- AMR1
- 2004: histologic features of AMR confirmed by positive immunofluorescence or immunoperoxidase staining for AMR (CD68, C4d)
- 1990: immunofluorescence, vasculitis, severe edema in the absence of cellular infiltrate
- histology
